You’ve been waiting for the appointment with the pediatric ophthalmologist to discuss your strabismus surgery for days or weeks with nervous anticipation. But when the surgeon walks in the door, your mind blanks and you forget all of the questions that you wanted to ask and just listen to them tell you that things went great and it should all sort out over the next few months.
You get home completely frustrated with yourself, still feeling confused.
In this article we will dive into the details of the questions you can ask at your post-surgery appointment that will leave you feeling confident instead of frustrated!
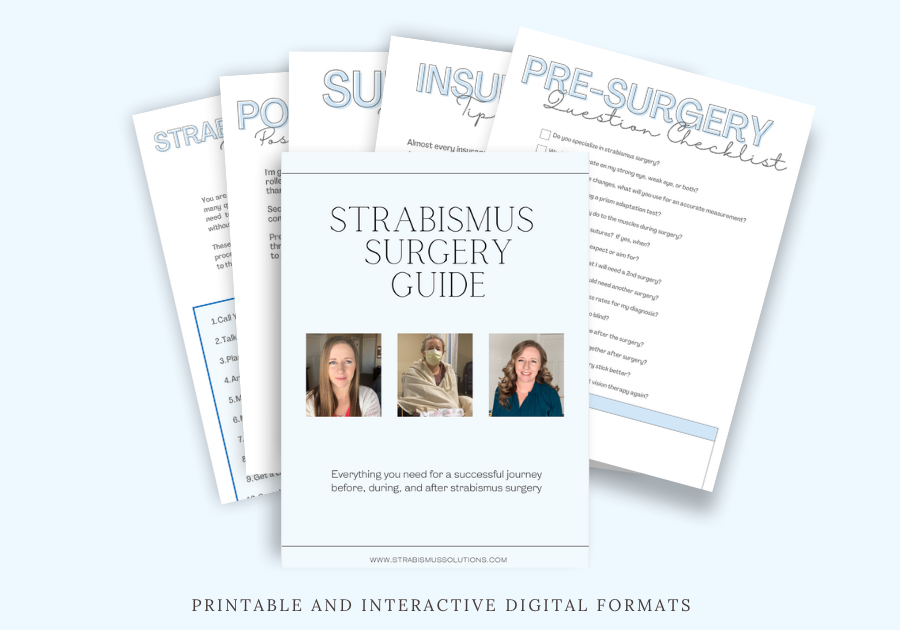
If you are a list person who likes to check boxes, I have something exciting for you. I’ve created a Strabismus Surgery Guide that includes checklists and information for insurance, pre and post-surgery appointments, packing lists and emotional help. It has 6 different areas where I will help you completely prepare, endure and recover from your surgery with confidence in both a printable and interactive digital format.
If you want to read about my personal experiences with strabismus surgery, you can find all of that information over HERE.
Keep reading for the extended explanations for questions that you can ask your surgeon at the post-surgery appointment.
15 Questions to Ask at the Post-Surgery Appointment:
What were my measurements before surgery?
Before surgery, careful measurements of the angle of your eye turn are taken by the orthoptist and ophthalmologist. You may have been esotropic, exotropic, hypertropic, or hypotropic. This is usually measured in prism diopters and usually ranges from 10-60 diopters before surgery. You may have different measurements at near and in the distance and have one number for a horizontal deviation and a second for a vertical deviation.
Get this information and write it down!

What are my measurements now?
Next, ask for your current measurements.
Knowing these measurements can help you see the changes that have occurred and help you understand visual symptoms you are experiencing.
You may be second guessing results and obsessing over how your eyes look at this point, having some facts to work with can help you avoid a complete spiral and mental breakdown. Keep it factual.
Would you consider this surgery a success?
You may be surprised to learn that even if the eyes aren’t perfectly straight, the surgery is still considered a success. You can bet that I considered my before/after a success, even though the alignment wasn’t perfect!
Understanding your surgeon’s qualifications for success will help you understand their plan for moving forward.
When can I expect the full results of the surgery?
Depending on the type of surgery, type of strabismus, adjustable sutures, number of muscles operated on and fusional abilities, the results after surgery can continue to change for weeks and months after the operation.
According to my surgeon, after about one week you get the basic idea of whether the surgery worked or not. Physical changes with eye position after that point aren’t as drastic. This isn’t true for the brain. The brain continues to adjust to the new position over the course of several months.
For me, my alignment continued to improve over a 6 month period.

How long do you expect the results to last?
Your surgeon has performed thousands (hopefully) of surgeries and will know better than anyone what to expect long-term. Strabismus brains and eyes are usually changing very frequently so having an idea of what to expect can help avoid some major frustrations down the road.
Would you recommend another surgery? If so, how long do I need to wait between surgeries?
If you are not within 10-15 diopters of being straight, your surgeon may recommend another surgery. Sometimes, especially with esotropia, multiple surgeries are needed to zero in on the target.
Some surgeons want to wait a full year to see how the eyes adjust over time, others are ready to jump in 3 months later. Each surgeon has a different philosophy here so try to understand why they do what they do. Are they hoping that your double vision eases over time? Do they think the over-correction is going to relax into place?
These things are possible, but case specific.
What is the maximum number of eye surgeries I can have?
This is the million dollar question. If in a surgery only one muscle is tweaked, that is much different than having 4 muscles cut, folded and reattached drastically. Having multiple invasive surgeries is different than multiple tweaks.
After surgery, your surgeon will be able to understand more about what is happening with your muscles. Is there scar tissue from previous surgeries? Is there room for further adjustments?
These things can only be seen when they are in the surgery room so they are great questions to ask afterwards.
If you did another surgery, what would you do differently to ensure a better result?
You can’t do the same thing over and over and expect different results. Follow-up surgeries are usually different, but this is a question that can help you decide whether another surgery is a good idea. It can help you decide if you trust your surgeon. Try to understand where they are coming from.
What can I do to help adjust to the new eye position?
After surgery, many people feel nauseous, dizzy and even have some double vision as their brain is learning how to use the eyes in the new position. This is completely normal and should be gone after several weeks, but that doesn’t make it any more comfortable.
Are there eye exercises, relaxation techniques, peripheral vision strategies, etc that can help my brain?
How long will the double vision/visual confusion last?
As they do their post-surgery check up and take a look at your eye position, fusion, and stereopsis, the surgeon is going to be able to help you understand why you may be experiencing some of these side effects. Understanding where it is coming from can help you know how to alleviate the symptoms and will give you and your surgeon a best guess of how long they will last.
If my eyes work together, will the result last longer?
If your eyes are fighting each other, do they actually want to be straight? Will they stay straight longer if you are getting fusion between the eyes. I definitely think so and I have experienced this, but what does your surgeon think?
He has literally seen into your eyes and can offer insight into this complicated process. He may not believe fusion is possible for you, but take him to the land of make believe and say that if a miracle occurred and you had perfect fusion, would your eyes stay straighter.
Do you have a vision therapy office that you recommend for post-surgery rehab?
If you have a knee surgery, you do about 30-40 post-op visits with a physical therapist to rehabilitate your knee and get it working again. The same thing is possible for your vision. In almost every case of strabismus, improvements can be made to your binocular vision which can help the results of surgery to stick. Many surgeons are very anti vision therapy, unfortunately, but it is a good subject to bring up and discus.
If your surgeon has a favorite optometrist that practices vision therapy and sends you there, you have found a gem and I need you to email me their information so I can spread the word. Most of them will need a little gentle prodding here.
When will the redness be gone?
You probably won’t forget to ask this one because it may be the item on the forefront of your mind since you’re seeing it in the mirror everyday. In general, the bulk of the noticeable redness will die down after two weeks. By week 4 it will hardly be noticeable and by 6 weeks you should be completely fine.
If you are dealing with any complications like infection, it may extend the healing time and your surgeon can help you sort out that timeline.
You can see that the redness hangs on for quite a while in my pictures below!

Are there signs to watch for in case of infection?
Noticing an oncoming infection can help you get it treated and back to normal before things get out of control. Know the signs to watch for and get a prescription ahead of time or communicate with your doctor the easiest and quickest way to get help if you were to get an infection.
Being proactive is going to help you feel more relaxed and confident which will make the whole process even easier.
When can I resume normal activities like swimming, makeup, lotions, contacts, etc?
Usually, surgeons say 2 weeks, but you may have a unique case so make sure to ask your surgeon directly. If you don’t, I can promise you’ll be searching google for the answer later on, but the best thing is to get the answer directly from the surgeon.
Wrap It Up
Each of these questions is going to help you understand what to expect and help you stay factual during this emotional time of getting strabismus surgery. If you would like to meet with me over zoom, I offer consultations and coaching for adults with strabismus (link below)
To get the amazing digital PDF I created to help you keep track of everything you’ll need for your surgery, use the link below.
